Blog Posts

Michelle's Story
"What's wrong with mummy?"
Michelle had always been the life of the party. A binge drinker, sure, but not someone who drank every day. Not someone with a "real problem." At least, that's what she told herself - right up until the night her daughter asked a question she couldn't ignore.
Michelle had just arrived home from a beer festival - but the problem was, she couldn’t remember how she got there.
She knows her friends brought her back - they must have, because she woke up in her own house. She'd arranged for someone to watch the kids, and she'd thought they'd be asleep by the time she arrived.
But they weren't.
Her daughter was old enough to ask questions. Old enough to remember when her father had struggled with his drinking, whose relationship with Michelle had ended years earlier. Old enough to see what was happening now and connect it to what had happened then.
"What's wrong with mummy?" she asked.
Soon after, the babysitter had to leave. Michelle was alone with her children, still intoxicated and still barely functional. "Who knows what could have happened," she says now, her voice quiet.
"You think about these things after the fact, and it's pretty shocking."
That moment of her daughter's question cutting through the fog, the memories it dragged up, the realisation of what could have gone wrong - that was the wake-up call she couldn't ignore anymore.
I wasn't a stereotypical 'alcoholic'
Here's the thing Michelle wants you to understand: she never thought she had a real problem.
She'd been drinking since before she was old enough to legally buy alcohol - always the life of the party, always fun and always up for it. A binge drinker, sure, but not a daily drinker. And that distinction mattered to her.
"I wasn't a stereotypical 'alcoholic,'" she explains.
"They call it grey area drinking. I wasn't drinking every day. I wasn't waking up and drinking first thing in the morning."
Michelle knows now that it’s easy to hide in that grey area. Easy to convince yourself you're fine because you can always point to someone worse and say, "At least I'm not that bad."

For years, Michelle stayed fairly stable with her drinking - but then loneliness crept in, life working from home got isolating and the stress built up. And her drinking, which had always been there in the background, started taking up more space in her life.
She told herself it helped. Stressful job, stressful single parenting - all the reasons you think a few drinks will take the edge off. "But it doesn't actually help," Michelle says now. "It just doesn't."
Still, she thought she needed it. More than that, she thought she enjoyed it. The idea of giving it up felt impossible, unnecessary even. She wasn't that bad.
Except the warning signs kept piling up.
The blackouts started adding up
First, there was the polo event.
One of those big day-drinking affairs where everyone's having a good time, the sun's out, the drinks are flowing. Michelle was there with all her friends, laughing and socialising, feeling fine.
Until somehow, they lost her.
She doesn't know what happened. Massive blackout. The next thing she remembers is being alone, trying to figure out how to get home. When she checked her wallet later, she found a card from a safety volunteer who'd helped her find her way.
"Pretty horrible," she remembers. "The anxiety the next day, the regrets, beating yourself up over it." Her mental health wasn't great to begin with, and these incidents weren't helping.
There were other nights where she didn't know how she got home. Little injuries she couldn't explain - nothing massive, but enough to make her wonder. Situations that, looking back, weren't safe. The kind of things you brush off in the moment but that stick with you later, nagging at the edges of your mind.
And then there was the beer festival - another day-drinking event with friends. Another afternoon that should have been fun.
She arrived home with no memory of the trip. Her daughter saw her in that state. Asked that question. And suddenly, Michelle couldn't brush it off anymore.
"That was probably what led up to me seriously thinking that something needed to change," she says.
The four month break
Not long after that night, Michelle was scheduled to have a planned surgical procedure. Her medical team outlined one key requirement: no alcohol. Her liver needed to shrink before surgery, and she couldn't drink during recovery either.
So she stopped - for four whole months.
"I did okay because it was a medical requirement," Michelle explains. When there's a rule, a reason, a deadline - she could stick to it. Four months alcohol-free. No problem.
She had the surgery, she recovered and life moved forward. But once the medical necessity had lifted, the drinking slowly crept back in.
Except this time it looked different. She wasn't going out to parties or festivals anymore. She was drinking alone at home, and working from home made that dangerously easy.
She'd try to set limits for herself, like only buying a six-pack, but then it was so simple to just order more and have it delivered to her door. "So that didn't always work," she says. "And then the weekends were a free-for-all."
But it wasn't just affecting her anymore.
"It wasn't a life for the kids. I wasn't there for them."
That realisation sat heavy in her chest. The pattern she'd sworn she'd never repeat was repeating itself right in front of her children's eyes.
Taking the first step
Michelle remembers seeing an ad for Clean Slate pop up on her Facebook feed. At first, she scrolled past, but then she saw it again. She clicked through, did some research, read what people were saying about it, and saw that her health fund covered the program.
But what Michelle liked the most, was that it didn't feel like “going to rehab”. There wasn't that stigma, that sense of "this is for people whose lives have completely fallen apart."
"It was actually easier to go ahead with it," Michelle explains. "I was still at home. I didn't have to find alternative care for my kids. Everything was done via telehealth, appointments were easy to book - and honestly? That convenience mattered."
The convenience wasn't just practical. It was psychological.
"There was less chance of backing out because it was so easy. And I could just be in my own home, in my own bed."
You have to do the work
Michelle figured out early that stopping drinking was only the first step.
"You have to do the work," she says, "otherwise nothing's going to change. I realised that pretty early in the piece."
Once Michelle had gone through her supported detox, the regular appointments with her nurse provided accountability. "It was good to have someone to be accountable to and to check in on how things are going and talk through any issues that have come up," she explains.
Then there were the group meetings which provided a sense of connection and community. Michelle explains, "it was great to connect with people that were going through the same process and having similar mindsets around alcohol - because other people don't always understand."
They also became a safe space to figure out how to live her life without alcohol as a crutch, because stressful things still happen, and difficult emotions still come up.
"I had a friendship breakdown after I gave up," Michelle shares. "Things like that - you don't always know how to navigate them. But you can talk through them in these meetings with other people who may have had the same situations. It's a safe environment."
What struck Michelle was how the telehealth format let her work through real challenges in real-time. She wasn't removed from her daily stressors - she was learning to handle them without alcohol.
But she's clear about this: none of it works unless you actually do it.
What's different now
When Michelle talks about what's changed since she stopped drinking, she doesn't speak in vague terms.
"You don't realise how much you spend on drinking."
All that money that used to disappear into bottles and deliveries she barely remembered ordering - it started accumulating instead. Becoming something she could actually use.
Her physical health improved, and she even quit smoking three and a half months into her journey.
And that confidence showed up at work too with Michelle negotiating a higher-paying job, something she's not sure she would have had the courage to do before. "I'm doing a lot better in my work now," she says.
But it's the bigger life shifts that really illustrate how much has changed.
Michelle bought her first house.
Something that felt completely out of reach when she was spending money on alcohol, when her focus was scattered and her confidence was low.
"I mean, it didn't all happen just because I quit drinking," Michelle is quick to clarify, because she knows how it sounds, how it might seem too good to be true. "But it culminated. And giving up alcohol definitely helped in that regard."

And then there's the shift that matters more than any house, job or amount of money saved: she's now present with her kids. Actually there, not just physically in the room but mentally and emotionally available.
"I'm more present with my kids. They're happier," Michelle says, and you can hear how much that means to her. "I'm looking after their health now, too."
Nine months into her journey, Michelle is clear about her intentions: "I'm 9 months alcohol-free now and don't intend on going back - because I don't need it."
What's the worst that could happen?
When Michelle is asked what she would say to someone who’s worried about a life without alcohol, her answer is characteristically direct:
"What's the worst that's going to happen? You get healthy, you save money. There's no downside I can see."
Before she quit, she thought she needed alcohol. Believed it was helping her cope with the stress of single parenting, the pressure of work, the loneliness - all of it. Those were the stories she told herself - that alcohol was a reward, a stress reliever, something she enjoyed that helped take the edge off.
"But it doesn't actually help," she says now.
It took those wake-up calls to make her see that her relationship with alcohol wasn't what she'd convinced herself it was. But here's the message Michelle wishes someone had told her years ago:
"You don't have to be the atypical or stereotypical ‘alcoholic’. I knew I had an issue with my relationship with alcohol, but I wasn't the stereotypical ‘alcoholic’." She pauses, making sure the words land. "Grey area drinking - I wasn't drinking every day, I wasn't waking up and drinking first thing. Doesn't mean you can't get help with the impacts alcohol might be having on your life."
"You don't have to hit rock bottom. I had a few rock bottoms along the way, and they definitely give you wake-up calls. But let's not go all the way to the bottom."
You don't have to lose everything to deserve help. You don't have to fit a narrow definition of "bad enough" either. If alcohol is impacting your life, your relationships, your parenting, your health, your sense of self - that's enough.

Shellie's Story
The party she never thought she'd have
Shellie spent an hour hiding out the back before her 60th birthday party began. She was nervous. Anxious. Convinced that maybe ten or fifteen people would show up - if that.
When she'd told friends she was planning a party, her first thought had been: Who will I invite? No one will show up. But the RSVPs kept coming. Ten became twenty. Twenty became forty. By the time the day arrived, sixty people had said yes.
There was something else unusual about this party: it was completely dry. No alcohol.
"It's not often you go to a dry party," Shellie says. "I felt guilt about it - how can I say people can't drink at my party? But people kept telling me, 'It's your party, you do what you want.'"
Standing in front of those sixty people - some who'd known her for 45 years, some who knew her whole story - Shellie made an announcement: she was also celebrating a year of sobriety.
"Some knew in the room that I was on that journey and some didn't," she remembers. "But it was just so empowering to be in that space without alcohol, with so much love and fun and good times."
What Shellie discovered that night was something she'd feared would never be true: people loved her for who she was. Not for being fun at the party. Not for having a drink in her hand. Just for being Shellie.
"I thought if I took the drink out of my life and I wasn't fun at the party, I would have nobody," she says. "But they still love me for who I am."
The bottle was her best friend
For most of her life, that hadn't felt true at all.
Shellie started drinking at 12. By her late fifties, she was a binge drinker - a bottle of vodka in a night, alone, in isolation. She didn't drink every day, and for years, that's how she convinced herself she didn't have a problem.
"I always made allowance for myself that I don't have a problem because I didn't drink every day," she explains. "But my biggest fear is when I do drink, I can't stop."
The bottle became, as she puts it, her best friend. It helped her cope with emotions she didn't know how to handle. It quieted the anxiety that made social situations unbearable. It numbed everything.
"When I have a drink, everything just goes away. It's a miracle," Shellie says. "I don't have to stress or worry about anything. But then it's the after effects - the impact it has on the quality of my life."

Those after effects were severe. Shellie lives with bipolar disorder, anxiety, and depression. For years, her drinking and mental health crises fed into each other in a relentless cycle. Life stressors would trigger binges, and binges would trigger mental health episodes.
"You put the two together and they just feed into each other," she says.
Her children had been on this journey with her since they were born. They'd seen the hospital visits, the relapses, the disappointment and worry. Shellie carries the memory of her son's face when she told him she'd started drinking again.
"The disappointment I saw in his eyes really broke me," she says. "As much as he was supportive and said, 'Mum, what are we going to do about this?' - just seeing that disappointment... those are all little snippets that stay in my head to remind myself not to pick up again."
She'd tried to get help before. Seven years earlier, after losing her mum, she'd spent six weeks in an inpatient rehab over Christmas - "one of the hardest things I've done." But she'd left saying she'd drink socially again.
"Which I can't drink socially and I can't drink at all," she says now.
The cycle continued. When her GP suggested connecting her to alcohol and other drug services, Shellie walked out.
"I said to her, 'I don't have a problem. I don't know what you're talking about,'" she remembers. "My picture of an ‘alcoholic’ was someone sitting in the gutter or down a laneway drinking out of a paper bag. I used to always go, 'That's not me. So I don't have a problem.'"
"Nanny, you were very silly last night"
It was her grandson who first planted a seed of change.
Shellie had started spending more time with her daughter's family, where weekend drinking was acceptable and normal. She was fun, laughing, the life of the gathering. Until one morning, her grandson looked up at her and said: "Nanny, you were very silly last night."
"That really touched me," Shellie says. "I thought, I need to be a nanny and a role model to my grandchildren."
But the real catalyst came on a camping trip with her daughter's family. Shellie drank so much that she nearly fell into the fire, and then she blacked out.
"That was my scary turning point," she says. "I could have fallen into the fire. Imagine how much my life would be different. I may not even be here."
That image stayed with her. As did another growing fear: she was getting older. Recovery from binges was taking a week instead of a day. She lived alone. What if she fell? What if she hurt herself and no one found her?
"As you get older, if that was to happen here at home on my own and I was to have a fall or knock myself out or break a hip - who's going to find me?" she explains.
Approaching 60 became a moment of reckoning. Shellie found herself asking: how do I want my life to look for the future?
"I choose not to drink again"
When Shellie's therapist from Mind Australia mentioned Clean Slate Clinic, Shellie went online and completed the suitability test. She was 59, scared, and still telling herself she didn't really have a problem.
But she reached out anyway.
"That fear - I always go back to that memory of falling in the fire," she says.
By the time she connected with Clean Slate, Shellie had already stopped drinking. The camping trip had frightened her enough that she quit on her own, determined not to start again. This meant she didn't need the formal detox week - instead, those check-ins became additional support time with her nurse.
"What I found is the program is flexible to your needs," Shellie says. "It's not a one-box-fits-all program."
From day one, Shellie was matched with Carol, a nurse who would stay with her throughout her entire journey. And something about Carol made all the difference.
"Carol's background and her experience made a big difference," Shellie explains. "I just saw her belief in me - the belief that she had in me that I would get through," Shellie says, her voice catching. "She held that torch of hope where I didn't hold that myself. I just thought, you know, I've done this my whole life, it's just going to be another cycle."
Carol became Shellie's cheerleader, celebrating milestones when Shellie couldn't celebrate herself because she was too afraid of failing again. The appointments gave Shellie something else she desperately needed: accountability.
"I don't want to hop on the screen and let anyone down," she says. "And knowing that I have an upcoming appointment, I can get things off and out of my headspace. It gives me the opportunity to look at things in another light, and then I go away and reflect and try to bring that into my life to move forward."
Shellie also started using the "I Am Sober" app, setting mantras and goals. Her mantra this time was different from seven years ago. Not "I'll drink socially again." This time: "I choose not to drink again."
The program worked around her life. Appointments were flexible. She could do everything from home, allowing her to work through her daily stressors as they came up.
"These stressors in life - we're in them every day," Shellie says. "By doing the program online, I could live and cope with all those stressors - rather than having to face them on the other side of my treatment.”
Discovering the other side of the fence
Shellie has a metaphor for what her life feels like now versus before.
"I spent my life on the side of the fence where the grass was dry - drought season," she says. "But now I'm on the other side of the fence where the grass is greener, the flowers are popping, the rainbows are out. Can you imagine that vibrance? That's just how my life is now."
Fifteen months alcohol-free, the changes are both profound and practical.
The brain fog is gone and her memory has improved immensely. She used to struggle to remember names, but now "there seems to be a lot more space up there to retain information." She's working three days a week. Her health and fitness have improved. And most importantly, she finally feels in control of her mental health.
"I'm a lot more balanced than what I have been," she says. "Bipolar is chaotic already, and when you put the drink on top of that, it just explodes. But now I'm quite balanced. I'm engaging in life, I'm being a mum and a nanny and a good friend."

The emotional shift is perhaps the biggest change.
"I'm now experiencing the positive emotions of life," Shellie says. "Before it was all black and grim. But now I can see joy and happiness and fun."
She's also proud of herself in a way she's never been before.
"I would always go through life feeling worthless and helpless and unloved and minimised," she says. "But today I'm proud of myself. I'm proud that I can be there as a mum and as a nanny to my grandchildren. I'm a lot more present."
When her son and his partner announced they were expecting a baby, they said something that stays with Shellie: "It's even more reason to stay sober."
"That's always in the back of my head," she says. "As much as I'm doing it for me, the drain it puts on the family when I ring them up and say I've started drinking again..."
She trails off, then adds: "I want to live today. There were many times throughout my life where I didn't want to live, but today I want to live. And I'm living a sober, happy, healthy life now."
"You have to be brave"
When Shellie thinks about what she'd say to someone considering reaching out for help, someone who's scared of what life might look like without alcohol, her message is straightforward.
"You have to let down your barriers and be humble," she says. "There is help out there, and it's okay to get help. The people you're getting help from have the professionalism and the knowledge. They can teach you so much that can assist you on your journey. But you can't stay stuck where you are and not have quality of life without trying."
She also wants to challenge the narrow picture of what addiction looks like - the same picture that kept her from getting help for so many years.
"I used to think an ‘alcoholic’ was someone in the gutter with a paper bag," she says. "That's not me, so I don't have a problem. But I was a high-functioning binge drinker. I didn't drink every day, but when I did drink, I couldn't stop. You don't have to fit that stereotype to need help."
For older people especially - people in her generation - Shellie wants them to know they're not alone.
"You don't hear stories about people like us - it's more the younger ones," she says. "But in our generation we go through a lot of stressors too. Kids move on. There's loneliness. You're feeling isolated. Your body changes as you age. It's okay to reach out."
She also emphasises something that was critical to her own recovery: addressing mental health and addiction together.
"Mental health and addiction - the two come together," Shellie says. "If that stuff had been addressed early and looked into, my journey may not have been as chaotic. The two need to work together. There's enough stigma with mental health, but then you put addiction on top of that - that's more stigma. Let's remove the stigma and move forward and get the help."
Her final message is simple: "You have to be brave."
The torch of hope that Carol once held for her? Shellie's holding it now, too.

Lisa's Story
When normal life feels extraordinary
Lisa now walks to the beach every morning from her new place. It's less than five minutes away - the prettiest beach in town, she says. There's a nature reserve nearby. Her mum is there with her. Everything just... works.
"Everything I touch turns to gold," she told her nurse recently. She had to stop and think about that.
"At first I thought - I'm so lucky," Lisa says. "But I don't know if it's all luck. Now, when I look at the good things happening to me - it's normal. Good things can happen. It's just that because I was drinking, because my life was always chaotic or boring or blending into one... that was my normal."
Six months ago, Lisa's normal was very different.
When wine o'clock kept creeping earlier
By her mid-fifties, Lisa had what she now recognises as a high-functioning alcohol dependence - though she was in denial about it at the time.
She'd wake up in the morning saying, "This is it. This is the last day." She was still working full-time, still caring for her mum, still functioning. But life was becoming increasingly isolated and overwhelming.
"Now that I look back, it was probably the alcohol that was becoming overwhelming," Lisa says, "Or the alcohol consumption was making everything else overwhelming."
She was a home drinker and recalls having glasses of wine scattered around the house - in the bathroom, the bedroom, and anywhere else that had slipped her mind. If it was raining on the weekend, she'd look at the weather and think: That's the go-ahead for me to stay home and drink today.
"That justified my actions at that point in time", she explains.
In the meantime, wine o'clock was creeping earlier and earlier. Five o'clock became two o'clock, and then she'd be in bed by eight because she’d drunk too much. Then she’d wake up and do it all again.
"I was sick of waking up feeling sick," Lisa says. "I was sick of just trudging through days, waiting till five o'clock came so I could drink."
She also knew that her drinking was affecting her health, having received poor liver function results years ago. Lisa explains, "I was starting to get really lazy. My weight was fine, but I wasn't exercising. I was just... plodding through life."
The long shadow
Over a decade before, Lisa experienced a series of traumatic events. What followed were years of being in survival mode - hypervigilance, fear, and alcohol as the only thing that made her feel strong enough to keep going.
"At first I was using it to numb my emotions," Lisa says. "It felt good when I was drunk - like I could handle anything."
She was drinking till two in the morning, then getting up and going to work at four, running on adrenaline and alcohol.
She was jumping at everything, even running red lights out of fear.
"In the scheme of everything else going on, the drinking was under-appreciated," she explains. "Which I'm not blaming anyone for. And I don't blame myself either. But that was my turning point."
For many years, she carried that weight, and it would take time before she was ready to put it down.
Lisa had tried to quit drinking twice before in her thirties, doing seven-day inpatient detox programs.
"It felt like a bit of a holiday," she says. "Seven days with no alcohol, some exercise. I got a little bit out of it. But as soon as I got out, I went straight back to drinking." Lisa explains, "I was a home drinker, and my alcohol consumption had become so much of a habit, I needed to break that habit in the place where I was doing it."
The night everything changed
One night, after a few too many scotches, Lisa sat down at her computer. She'd been thinking a lot about what was going to happen to her, and she knew that she didn’t like the way her life was progressing.
"I just was sick of it," she says. "I was just ready."
She Googled something about alcohol support and Clean Slate Clinic came up. At-home detox. She read it and thought: That is me. That’s exactly what I need.
She completed the suitability test and booked a call for 8:45am the next day.
"I thought, 'Yeah, this call sounds good,'" Lisa remembers. "Then I woke up thinking, 'Crap, what have I done?’"
But that immediate follow-up call changed everything.
"It didn't give me that second chance to back out," she says. "And it certainly opened my eyes up when I was sober."
After speaking with Andrew, a lived experience member of the Clean Slate team, Lisa finally felt like someone understood what she was going through - and she realised that she was ready to make a change.
"I'm more scared about what life will be like without it"
Lisa told her family and friends about starting the program, feeling excited (and terrified).
"Everyone was overwhelmingly supportive," she says. "They kept asking, 'Are you scared?' And I said, 'Yeah, I am scared. I'm more scared about what life's gonna be like without it than actually doing the detox.'"
She visited her daughter before starting the detox, planning to go out with a bang. But something had already shifted.
"I hardly drank anything. But when I did, I was really quiet and I was present," Lisa says. "My daughter just said, 'Wow.' Even when she offered me wine at two o'clock on the weekend, I'd say, 'You know what? I don't even feel like one.' I was already working on it - it was just coming naturally for me."
When she got home, she started the preparation phase of the program. And within two weeks, she’d had an epiphany and decided to retire and move interstate.
"There were really, really good barriers," Lisa says. "But I looked at my life and thought: the ducks need help lining up. You have to pull them. You can't just wait."
Going from strength to strength
Lisa then went through her detox at home while packing up her entire life.
On day one, she put her Fitbit back on and started exercising again - something she hadn't done in years. She set goals every night for the next day. She dealt with the stress of relocating. And she just managed it.
"I just took control," Lisa says. "I just did it."
She now plays simple games with her mum every night, like Scrabble, and they laugh until they cry. "We haven't laughed so much in years," Lisa says.
Sometimes when they're doing something together, Lisa tells her mum: "You know what? I wouldn't have been able to do this if I was drinking."
.jpg)
Lisa takes a moment to reflect, sharing, "Life was just too hard before; it had one massive, day-in, day-out barrier. And now that barrier's gone."
Lisa's relationship with her children has also changed completely, with both having seen her through tough times.
"When my son used to call me - I look back now and I think he was only calling because he felt he had to," Lisa says. "There was no real conversation, probably because he thought I'd forget - which I would. My memory was terrible. I'd have serious conversations at nighttime and have no idea the next day. Now when he calls me, it's just... different. It’s real."
"I'm double as good at everything I was scared of"
Lisa's biggest fear before quitting drinking was losing herself.
"I thought I wouldn't be funny. I wouldn’t be confident," she says. "I'll be the third wheel. I'll be the stick in the mud. I'll be boring. I won't want to go anywhere."
She laughs now at how wrong she was.
"I cannot be any further from the opposite," Lisa says. "I'm funny, I'm confident, I'm fit, I'm strong. And I'm still the life of the party."
She’s now replaced the scattered glasses of wine with green juice, sharing, "It wasn't because I was craving wine. It's just that every time I went to pick something up, I would think of wine. So I put green juices around instead."
From the minute she wakes up
"When people ask about my favourite part of the day, I say: from the minute I wake up, everything is my favourite," Lisa says. "I look forward to my walk, to getting home and having coffee, to going out for lunch, to my nap. I look forward to everything."
Lisa’s now been alcohol-free for six months. She's retired. She's living near her daughter and her grandchildren. She's caring for her mum. And she's at the beach every morning.

"I used to think this was a holiday," she says. "Like, I'd be doing something and think, 'I'll have to go home soon' - because in my head I was on a holiday. Then I’d have to remind myself, 'This is real. I live here.'"
Everything she touches turns to gold. But it's not luck. It's what happens when the barrier that made life too hard - the day-in, day-out habit that blended everything into one - is finally gone.
"Good things can happen," Lisa says. "It's just normal now. And normal feels extraordinary."
If this story brings up difficult feelings for you, or if you or someone you know is struggling, support is available. Please contact Lifeline on 13 11 14 (24/7) or visit lifeline.org.au.

How to Set Boundaries Without Guilt: A Partner’s Guide to Alcohol Dependence
At Clean Slate Clinic, we know recovery doesn’t belong to one person - it’s a journey that touches everyone around them. That’s why we spoke with Amanda Lockyer, addiction relationship coach and founder of Addiction Makes Three, where she helps partners and families of people with AOD dependence set healthy boundaries and rebuild self-worth. In our conversation, Amanda shared how clear boundaries can protect relationships, restore dignity, and ease the guilt that so often accompanies caring for someone in recovery.

Amanda describes the emotional weight many partners carry as “confusion wrapped in love.” Most people, she says, are desperate to help but unsure how. “They don’t know what’s helpful or what’s unhelpful. There’s grief for the life their loved one isn’t living - and grief for themselves, too. But there’s still hope.”
That hope often fuels what she calls rescue mode - the belief that you can fix what’s broken if you just try hard enough. From the outside, it feels like love in action; in reality, it becomes a cycle of exhaustion and control. When partners start rearranging their lives around someone else’s drinking, they slowly disconnect from themselves.
Signs you may be losing yourself
Amanda identifies several key indicators that you may be losing yourself in someone else's journey:
- Stepping back from connection
Withdrawing from friendships, hobbies, and activities that bring you joy
- Making yourself negotiable
Skipping meals, abandoning exercise routines, or neglecting morning walks
- Mental preoccupation
Their struggles become your first thought upon waking and last thought before sleep
- Identity erosion
Struggling to answer simple questions about your own preferences and needs
Recognising these patterns early creates space for change before exhaustion and isolation take hold.

Reclaiming your sense of self is the foundation for any healthy boundary. “You need to know who you are and what you stand for,” Amanda says. Many partners and family members lose this clarity in the chaos of addiction. Reconnection begins by returning to your core values, and using them as a compass for daily choices.
Boundaries, she explains, are not walls but bridges: an expression of self-respect that keeps connection possible. “A boundary says, ‘I love you - and this is how I love me too,’” she explains. Far from being cruel, boundaries are what make genuine support sustainable.
Setting boundaries can start small. You might decide not to answer phone calls late at night, or choose not to lend money while still offering to share a meal. The goal isn’t to punish your loved one - it’s to protect your peace.
The discomfort that often follows is normal. Guilt and fear tend to surface when you begin prioritising yourself after years of putting someone else first. But this isn’t a sign you’re doing something wrong - it’s a sign you’re learning a healthier pattern.
Letting go of control is equally freeing. “Control is an illusion,” Amanda says. “It comes from love, but it only fuels anxiety. What you have is influence - and influence is far more powerful.”
When partners and family members focus on their own wellbeing, they model the stability that recovery requires. Noticing and reinforcing small positive moments - a dinner shared, a conversation that ends kindly - helps rebuild trust. “Connection is the opposite of addiction,” she adds. “Those small moments matter.”
Practical tools to regain balance
- The litmus test for daily decisions
Each night, ask yourself: Can I go to bed at peace with the choices I made today? If yes, they were the right choices for that day. Tomorrow, you can make new ones. This simple reflection shifts focus from perfection to progress. - The square-inch of paper
“Everyone has opinions - like noses,” Amanda laughs. Write the names of the few people whose opinions truly matter to you on a square-inch piece of paper. Put your own name at the top. When doubt creeps in about a boundary or decision, return to that list. If someone’s not on it, their opinion doesn’t belong in the conversation. - Values as a lens
Reclaiming your sense of self starts with clarity on what you stand for - such as; kindness, integrity, calm, respect. Use those values as your filter for decisions. When choices align with your values, guilt softens because your actions reflect who you truly are. - Preparing for hard conversations
When boundaries need to be expressed, plan ahead. Focus on one issue at a time, lead with ‘I feel’ statements, and choose a calm moment to talk. “The power of the pause can save a relationship,” Amanda says. Take a breath - and if things become heated, step back rather than push through.

The key is to start small and build momentum. “Make one promise to yourself and keep it,” Amanda suggests. “Eat three meals a day, go for a walk twice a week, meet a friend for coffee. Every time you keep a promise to yourself, you remind your brain that you matter too.”
This simple practice can help restore self-trust - something often eroded in the chaos of addiction. It’s also a gentle antidote to guilt. Taking care of yourself doesn’t mean abandoning your loved one; it means ensuring you have the strength to support them when it counts. “You’re in crisis too,” Amanda reminds partners. “You deserve support just as much as your loved one.”
It’s a simple philosophy, but one that can transform families. “Partners and family members are struggling in silence behind closed doors,” Amanda reflects. “We feel forgotten. But when we start caring for ourselves again, we lead the way for change - in ourselves, our families, and our loved ones.”
Learn more about Amanda’s work at Addiction Makes Three.
Explore Clean Slate’s support person resources designed specifically for partners and family members navigating a loved one's recovery journey.

Sober For The Holidays
The holidays can be amazing, overwhelming, and a little unpredictable - sometimes all at once.
In this free webinar, we have a real, honest and slightly awkward conversation about what it’s actually like to move through the festive season without leaning on alcohol.
It’s a time filled with joy, pressure, family dynamics, back-to-back events, not enough downtime, and always someone saying, “Go on - it’s Christmas!”
Clean Slate’s Dr Chris Davis and Sober Awkward's Victoria Vanstone unpack the whole messy mix together with humour, honesty and zero judgement.
Speakers:
Dr Chris Davis | Clean Slate Clinic
Dr Chris is a GP, Addiction Medicine Specialist, and the co-founder & Medical Director of Clean Slate Clinic. With over 10 years of experience, he’s passionate about breaking down stigma, speaking openly about the things people often hide, and making support feel human - not clinical.
Victoria Vanstone | Sober Awkward
Victoria is the co-host of the Sober Awkward podcast and a passionate advocate for honest, alcohol-free living. After years of being the life of the party, she made the decision to quit drinking in her 40s and hasn’t looked back. Victoria brings humour, heart, and a refreshingly real take on sobriety - especially the messy, awkward bits.
Want more real, relatable sobriety stories? Check out the Sober Awkward podcast or join their online community at cuppa.community.
Holiday Support Options
If you feel like you need additional support over the holiday period, please contact your GP or psychologist. The below services also offer free & confidential care:
- ADIS 24 hour support line - 1800 250 015
- NSW Mental Health Line - 1800 011 511
- Lifeline Australia - 13 11 14
- Beyond Blue - 1300 22 4636
- MensLine Australia - 1300 789 978
- Kids Helpline - 1800 551 800
- Suicide Call Back Service - 1300 659 467
- 13YARN - 13 92 76
- 1800RESPECT for domestic violence support
An Interview with April Long
April is the CEO of SMART Recovery, one of our trusted partner organisations. Recently, we sat down with them to hear about their thoughts on addiction support sector.

Can you tell us a bit about Smart Recovery?
SMART Recovery is designed to support individuals seeking recovery from addiction and problematic behaviours. It provides a science-based approach to addiction recovery and offers tools and techniques for self-empowerment.
We train organisations and individuals to run their own SMART Meeting with their community online or in person. We currently have over 250 meetings around the Australia.
SMART Recovery Australia proudly stands as a secular champion of recovery, partnering with over 75 Member organisations nationwide to deliver more than 250 local recovery meetings.
We believe in acting locally while thinking globally, as part of a global community of 3000 mutual-support groups led by SMART Recovery International.SMART Recovery Australia reduces the time taken to seek help by addressing the traditional barriers associated with seeking and accessing help for addiction.
Can you tell us a bit about yourself?
I joined SMART Recovery as CEO just over 12 months ago. Prior, I had been working with children with a parent in prison at SHINE for Kids trying to reduce the impact of intergenerational incarceration and ensure healthy thriving families. I have seen a huge number of parents in custody who had not been given support but criminalised because of addiction, trauma and coping mechanisms that were not working for them.
I have my own lived experience of parental incarceration and addiction, and I am dedicated to supporting others on their healing journeys. I am driven to create a society that fosters support rather than stigmatisation.
What inspires you to do what you do every day?
What inspires me every day is my family and the courageous individuals who join SMART meetings to initiate the change they desire. I am motivated by those who, despite experiencing trauma, life challenges, and societal pressures, take that brave first step toward seeking a different path. Whether its attending a SMART Meeting, AA, undergoing home detox, or seeking residential support.
What do you see as the main benefits of home detox?
Home detox brings comfort, privacy, cost savings, and the ability to self-manage health with proper medical supervision. One of the most significant advantages is the comfort and emotional support it provides. Detoxification is a monumental step for most people, and being able to go through it in a familiar environment surrounded by their own comforts and support systems can make a world of difference.
What do you see as the potential of digital interventions and services in addressing addiction service gaps?
One of the key advantages of digital interventions is the increased accessibility they provide. Not everyone has equal access to in-person services, and digital platforms can bridge that gap. They reach individuals who may be geographically isolated or have limited mobility, offering them a way to access treatment and support from the comfort of their own homes.
The initial first steps in seeking help through digital platforms can be a powerful catalyst, leading individuals to pursue more intensive face-to-face treatment options if needed.
What other changes would you like to see in how we think about and treat addiction?
Addiction is not a moral failing. Some of the greatest people I know and love have been impacted by addiction. They are kind, successful, loving, have good values and morals. They work hard and they care about their family and their community. It is vital to understand that addiction does not define a person’s worth or character.
As individuals, we have personal responsibility for seeking help and making positivechanges. However, as a community, we share a collective responsibility to support and understand our brothers, sisters, aunties, and uncles who are facing addiction.
Instead of judgment and blame, we must offer understanding and support. By walking alongside them, we can foster an environment of empathy and compassion.To challenge the stigma and shame associated with addiction, we need to change public attitudes and beliefs. This requires open dialogue and the sharing of diverse experiences to help break down stereotypes and create a more inclusive and supportive society.
Policy reform is also necessary to create a more compassionate and supportiveenvironment for those affected by addiction. We should advocate for policies that reduce stigma, improve access to healthcare services, and prioritise a comprehensive approach to addiction treatment and support. This involves addressing systemic barriers, increasing funding for prevention and treatment, and ensuring that individuals can access the care they need without fear of discrimination or obstacles.
What do you see as the value or potential of your relationship with Clean Slate Clinic (to you / Smart Recovery)?
The primary focus of our partnership is to promote understanding, foster compassion, and ensure accessible and effective treatment for all individuals affected by addiction. People who are already falling through the cracks don’t need more gaps and a disconnected service system. By joining forces, Clean Slate Clinic and SMART Recovery enhance the support available, ensuring that no one is left behind.
What advice would you give someone who is looking to change their relationship with alcohol or another substance?
I want you to know that you are incredibly brave and capable. You are not alone in this journey. There are tools and support available to help you overcome the challenges you’re facing. I understand that the road ahead may be tough, but always remember that there is a community of people who have gone through similar experiences and are ready to offer their support.
It’s important to find what works best for you. Take the time to discover the strategies and resources that resonate with you personally. Set meaningful goals for yourself and work towards them. Remember, you have the power within you to change your thoughts, feelings, and behaviours. While urges and cravings may arise, you can learn to manage them with the right support and coping mechanisms.
This is your life, and your story should be written on your own terms. However, please know that you don’t have to face this alone. Reach out to those who understand and care about your well-being.
You are not defined by any addiction. You deserve a life of health, happiness, and fulfilment. Believe in yourself and take those courageous steps forward. You have a whole community standing beside you, ready to support you every step of the way.
What would you like to see from Clean Slate Clinic next?
As a priority, through digital innovation and collaboration I would love to see Clean Slate Clinic available in every community in Australia where support is needed.
Addiction is a global public health concern with widespread impacts and I see huge potential for Clean Slate Clinic and SMART Recovery to act locally and think globally.
Collaboration among governments, organisations, healthcare systems, and communities is necessary to tackle the challenges posed by addiction on a global scale and to improve access to support and treatment for individuals affected by addiction. I would like to see Clean Slate Clinic supporting that collaboration and scaling what works nationally to around the world.
Our national partnership will continue to help consolidate the alcohol addiction help space within Australia.
For more information on SMART recovery, visit this link.


Home alcohol detox: what actually happens
For many people, the fear of withdrawal is not about whether they want to change - it’s the uncertainty around what their body will feel like when alcohol is no longer there, and that fear is valid. If alcohol has been part of your coping system for years (or decades), the idea of stopping can feel like stepping off a cliff. But it doesn’t have to.
With a medically supported home detox, the process isn’t sudden or chaotic. It’s planned, paced, and monitored, with changes beginning long before your first alcohol-free day.

Phase one: the preparation stage
This part is often misunderstood as a waiting period. Lasting for approximately three weeks, this important phase is all about preparing your mind and body so that the transition is safer, calmer and more predictable.
During this time, you will be allocated your dedicated Clean Slate nurse who will be alongside you for the full program. Your first two nurse appointments will involve:
- Reviewing your medical history and drinking patterns
- Clarifying your goals and what you want this change to mean in your life
- Completing a risk assessment together, so you understand the safety plan
- Having blood and urine tests with your local pathology provider and later reviewing the results together
- Educating your support person on what to expect and how best to support you
- Confirming your detox start date and beginning to shape your recovery plan
You’ll also start using our daily drinks diaries to both record your alcohol use, and begin reflecting on your triggers, associations and the reasons behind your drinking. These are used for understanding what your nervous system has been relying on, so your medication, monitoring and recovery plan can be personalised.
Alongside this, you’ll have access to our digital resources that explore the neuroscience of addiction, the role of shame, goal setting and self-management strategies. These help your mind prepare for change in a way that feels grounded rather than abrupt.
You’ll also receive a care package that includes the essential Vitamin B1 (thiamine), our welcome letter and a breathalyser.
Before detox begins, you’ll have a review with your Clean Slate Doctor or Nurse Practitioner. Together, you’ll talk through your test results, confirm readiness and if clinically appropriate, medication for your detox week will be prescribed. Sometimes this includes diazepam - but only if your assessment indicates it’s needed. Craving reduction medication such as naltrexone or acamprosate may also be discussed for post-detox, depending on your goals.
By the end of these three weeks, you know what will happen and when, and the plan behind every step.
Phase two: detox week (the week without alcohol)
This is where your body makes the shift. Alcohol is suddenly no longer “holding the system together”, so the nervous system has to rebalance. While this can feel uncomfortable, it’s important to remember that it is temporary and you’ll be supported throughout the entire process.
During detox week, you will have daily appointments with your dedicated Clean Slate nurse where you will:
- Review your withdrawal symptoms
- Discuss medication adjustments (if needed)
- Check breathalyser readings
- Review your heart rate
- Receive psychological support and reassurance
You will also collect your medication from your local pharmacy on a daily basis and continue accessing our digital tools to support sleep, sensory regulation and early recovery.
What withdrawal usually feels like
Most people begin feeling symptoms within 12 to 48 hours. Common sensations include:
- Shakiness
- Sweating
- Nausea
- Anxiety or restlessness
- “Wired but exhausted” sleep
Symptoms usually peak around day 3 or 4, and gradually settle between days 5 and 7. Many people describe a moment towards the end of the week where things begin to clear - when they feel less foggy, less on edge, and more like themselves than they have in a long time.
At the end of this week, you will meet with your Clean Slate Doctor or Nurse Practitioner again to reflect, review, and discuss whether craving-reduction medication may be useful in the weeks ahead.
Phase three: why aftercare matters
Your body and nervous system continues to adjust in the days and weeks after detox - from sleep improvements to more regulated emotions, and of course, your mind starts to experience calm without alcohol being the gateway to it.
Having support in this stage makes a real difference, because maintaining recovery isn’t just about removing alcohol - it’s about understanding why alcohol has played such a dominant role, and building a life that feels easier to remain present for.
Importantly, phase 3 - the recovery and support phase - lasts for a full 12 months post-detox. This includes regular check ups with your dedicated nurse, online masterclasses each month and at least one recovery support group available to you every single day of the year. These evidence based SMART recovery groups have been proven to increase your chance of sticking to your goals in the longer term.

Final thoughts
If you’re reading this because you’re considering a detox, it likely means a part of you is ready for a different relationship with alcohol - or even a different relationship with yourself. You don’t have to do this alone, and you don’t have to push through uncertainty without support.
There is a safer, calmer, medically supervised pathway through this transition - and you can take your next step at a pace that feels right for you.
If you’d like to explore whether this pathway is right for you, simply check your suitability today.
FAQ's
Is home detox safe?
Absolutely, home detoxes are safe when they are medically supervised by experienced clinicians with screening, pathology, medication if needed, and daily monitoring.
How long does withdrawal last?
Symptoms usually begin within 12-48 hours, peak around day 3 or 4, and settle around day 5-7. Sleep can take longer to stabilise for some people.
Do I need time off work?
This will depend on your individual circumstances and initial assessment. Most people choose to take time off during detox week because symptoms and medication (if needed) can impact focus, decision-making and energy levels.
What medication is used during detox?
Some people are prescribed diazepam during detox if clinically appropriate alongside medications for nausea and other physical symptoms. Other medications such as naltrexone or acamprosate may also be discussed for relief from cravings after detox.
Can I detox without medication?
Yes - not everyone needs medication depending on their risk. Decisions are based on your individual clinical assessment, goals and safety.

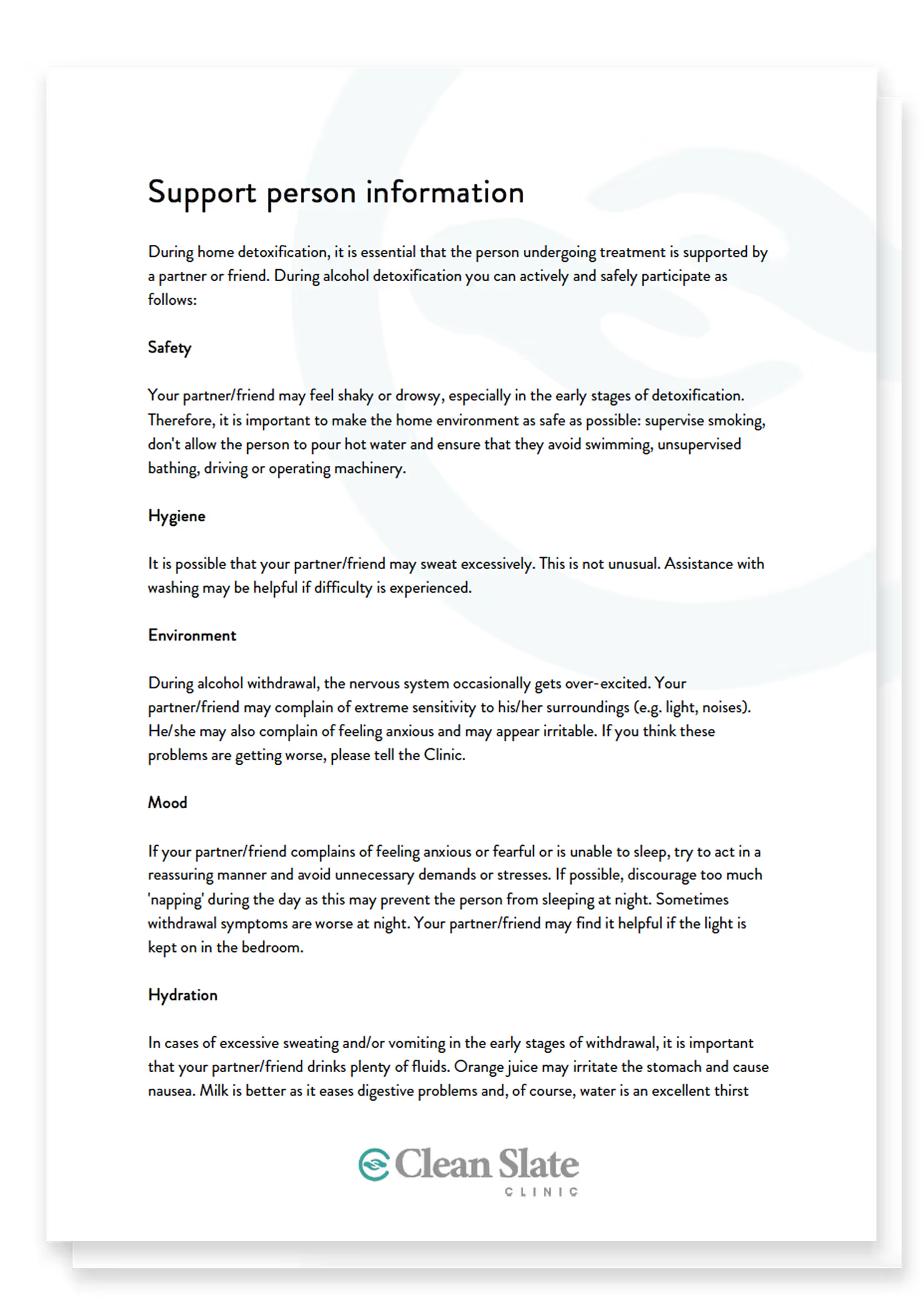
Support person information
During home detoxification, it is essential that the person undergoing treatment is supported by a partner or friend. Provide the following document to your chosen support person so they can actively and safely participate
For more advice or information please contact us
Download the PDF:
Clean Slate Clinic - Support person information.pdf
Download the Word doc:
Clean Slate Clinic - Support person information.docx
Preview:

Maintaining Motivation
The following questions are useful for people to reflect on in the maintenance stage of change to help them stay on track and keep up their motivation.
Download the PDF:
Clean Slate Clinic - Maintaining motivation.pdf
Download the Word document:
Clean Slate Clinic - Maintaining motivation.docx
Preview:

Pacing Skills & Self-Management
This document gives you some useful tips on how to practice mindful drinking and ideas on how to reduce or slow down your drinking, therefore helping prevent some of the associated harms.
Download the PDF:
Clean Slate Clinic - Pacing skills and self-management.pdf
Download the Word doc:
Clean Slate Clinic - Pacing skills and self-management.docx
Preview:

Pia's Story
Pia grew up in Guernsey and, like many of us, was introduced to alcohol at a young age. By the time she entered the corporate world, drinking wasn’t just normal - it was expected.
“Corporate culture celebrated burning the candle at both ends - work hard, play hard - but no one talked about the personal cost. The access to free alcohol was out-of-control. I could attend a booze-laden client or internal event every night - and was often expected to. Add to this the frequent travel, with airport lounges opening their bars up at lunchtime - next time you’re in an airport lounge mid-afternoon, look around - you’ll see dozens of men and women in corporate wear making repeated trips to the bar.”

On paper, Pia’s life looked perfect. A thriving career in healthcare consulting. Leadership roles. The kind of CV that sparkles. But inside, it was a different story.
“I was excelling professionally, ticking all the boxes, but internally I was struggling. Despite working in the healthcare industry for 20 years, I had no clue how or where to look for help.”
By late 2019, she was drinking 1-2 bottles of wine a night. Sometimes she hid it by pre-loading before events. Other times she poured white wine into a mug during Zoom calls so it looked like tea.
“I distinctly remember sitting in an afternoon Zoom meeting, drinking white wine from a mug and realising that this really wasn’t normal.” The shame was crushing. “There’s still so much stigma for professionals struggling with alcohol. It’s terrifying to think that being honest about it could cost you your career.”
For Pia, there was no dramatic rock bottom. No single incident that forced her hand. Instead, it was a series of quiet realisations - small moments that added up to a truth she couldn't ignore for any longer.
In 2020, after years of pushing herself to breaking point, Pia walked away from her corporate career. She and her fiancé packed up their lives, grabbed their dog, and set off in a caravan to explore Australia. At the same time, a piece of fate landed in her lap. Her best friend, Dr Chris Davis, asked if she’d help him get his virtual dependence treatment model off the ground. He had no idea that she was struggling with the exact same issue herself.
Testing the program was a wake-up call, particularly when Pia discovered that she met the criteria for a medicated detox. “That shocked even me,” she admits, now understanding the extent of her alcohol dependence. She then became “patient zero” in what would later become Clean Slate Clinic.

Pia went through detox and a full 12 months of aftercare. It wasn’t easy - recovery rarely is - but what surprised her most was how quickly the benefits began to appear.
“I knew I needed to stop, but I had this deficit mindset, which was ‘I need to stop because I’m tired of being tired, I’m scared of my increased cancer risk, I’m scared of my increased dementia risk, I’m getting older.’ I really hadn’t thought about the good stuff that would come. And there’s just so much good stuff, quite quickly as well. My anxiety, which was one of my main causes for picking up the bottle of wine every night, just disappeared. You feel this sense of control over your life. Life isn’t rainbows and unicorns all the time, but you can cope with everything so much better when you have clarity and good quality sleep.”
One of her favourite quotes sums it up with humour and truth: “I’ve never met a person who says they wish they’d stayed up later and drank more the night before.”
Today, Pia’s life feels grounded in purpose. She’s grateful for the unexpected chain of events that gave her the support she needed - support she didn’t know how to find, even after two decades in healthcare.
“I’m incredibly grateful for the serendipitous events that led to me getting the support I needed - I really don’t know where I’d be today had I not had that opportunity. I’m happy in the purpose I’ve found at Clean Slate Clinic - helping others in a similar situation brings me a lot of joy. Addressing my alcohol use has taken me on a journey of self-discovery that has brought me clarity, purpose and peace.”

She’s honest that life isn’t perfect. She still struggles with overcommitting and setting high expectations for herself - but now she has healthier ways to cope. Recovery didn’t erase life’s pressures, but it gave her the tools to face them head-on.
If you see yourself in Pia’s story, know this: recovery isn’t about what you lose - it’s about what you gain. Better sleep. Less anxiety. More peace. A sense of control you might not even remember having.
“There’s so much good stuff on the other side. I never expected that. And I wouldn’t trade it for anything.”

The Truth About Alcohol and Anxiety: What You Need to Know
“Why does that glass of wine feel like it helps... but then makes things worse?”
Picture this: It’s the end of a long day and you just want to relax - quiet the nerves, calm the mind, and slow the racing thoughts - so you have a drink (or a few). And in that moment, it works. Alcohol can bring a temporary sense of ease as the tension softens, the body relaxes, and everything feels a little more manageable.
But then comes the flip side. That wired-but-tired feeling in the middle of the night. The vague sense of dread in the morning. The sharp rise in anxiety a day or two later, often without a clear cause. Over time, many people start to notice that the thing they’re using to manage their anxiety might actually be making it worse.
If that sounds familiar, this post is for you.

Why alcohol feels like a friend (briefly)
Alcohol has a sedating effect on the brain. It increases the activity of a neurotransmitter called GABA - your brain’s natural “calming” chemical - this dampens the activity of excitatory chemicals like adrenaline, cortisol and glutamate. That’s why a drink can make you feel relaxed, sleepy, or even euphoric in the moment. It’s your nervous system temporarily slowing down.
But here’s the catch: your brain is always trying to maintain balance. When alcohol is regularly introduced, your brain starts to adapt by turning down GABA’s calming effect and ramping up excitatory activity to compensate. So while alcohol might feel like it’s “helping” in the short term, it’s actually setting the stage for more stress, more reactivity, and more anxiety once it wears off.
One way to think of it is this: alcohol lets you borrow calm from your future self - but with interest. And that interest gets steeper the more frequently you borrow.
When the hangover is more than physical: the anxiety rebound
This is where things start to feel more confusing for people. Because the anxiety doesn’t always show up right away.
In the hours and days after drinking - especially after heavier use - your brain chemistry swings back in the other direction. GABA activity drops further. Glutamate spikes. Your nervous system enters a state of high alert, often without warning. This can look like:
- Restlessness or agitation
- Feeling like you can’t catch your breath
- Trouble sleeping (especially waking in the early hours of the morning)
- Racing thoughts, irritability, or panic for no clear reason
A 2020 study found that people often experience peak anxiety symptoms 12-48 hours after drinking - even in the absence of a hangover. This is sometimes referred to as “hangxiety,” and it’s more than just a catchy term. It’s a sign that your brain is in recovery mode, trying to reset its balance after being artificially altered by alcohol.
If this sounds like a loop you’re stuck in - relief, rebound, repeat - you’re not broken. You’re human. And your brain is doing exactly what it was designed to do.
So, how can you manage anxiety without alcohol?
There’s no one-size-fits-all approach, but here’s the good news: it’s absolutely possible to feel calm, grounded, and in control without using alcohol to get there. Here are a few strategies we’ve seen make a real difference for our clients:
- Support your nervous system: Simple practices like deep belly, or ‘diaphragmatic’ breathing, gentle movement, warm showers, or grounding techniques (like holding ice or standing barefoot outside) can help calm your system when anxiety flares.
- Sleep, food and hydration matter more than you think: Disrupted sleep, low blood sugar and dehydration can all mimic or worsen anxiety. Try to stabilise your sleep routine, eat regularly, and keep your water intake up - especially if you’re cutting back on alcohol.
- Reduce other stimulants: Caffeine, high-sugar snacks, and even scrolling TikTok before bed can overstimulate your system. Pulling back a little can give your nervous system a break.
- Talk to someone: Whether it’s your GP, a therapist, or a service like ours - having someone who can help you build a personalised plan is incredibly valuable.
- Give your brain time: Research shows that even after just 2-4 weeks without alcohol, many people report reduced anxiety and improved emotional regulation. The longer the break, the more time your brain has to re-balance itself.
You don’t have to do all of this at once. Start where you are, with what you have. Small steps matter.

Final thoughts: The loop can be broken
Alcohol might feel like the quickest fix for anxiety, but over time, it often creates the very thing it promises to relieve. The good news? You can absolutely interrupt that pattern. And you don’t have to do it alone.
At Clean Slate, we can help you understand what’s going on in your body and brain - and build a plan that feels realistic, safe, and supported. If you’re feeling caught in the cycle, you’re not failing - you’re just ready for a new way through.
Check your suitability today.
Sources
Brousse, G., Arnaud, B., Vorspan, F., Richard, D., Dissard, A., Dubois, M., Pic, D., Geneste, J., Xavier, L., Authier, N., Sapin, V., Llorca, P-M., De Chazeron, I., Minet-Quinard, R. & Schmidt, J., 2012. Alteration of glutamate/GABA balance during acute alcohol withdrawal in emergency department: a prospective analysis. Alcohol and Alcoholism, 47(5), pp.501–508. [online] Available at: https://academic.oup.com/alcalc/article-abstract/47/5/501/99762?redirectedFrom=fulltext
Nutt, D.J. & Nestor, L.J., 2018. The GABA system and addiction. Addiction. 2nd ed. Oxford Psychiatry Library Series. Oxford: Oxford University Press. [online] Available at: https://doi.org/10.1093/med/9780198797746.003.0008
Kushner, M.G., Abrams, K. & Borchardt, C., 2000. The relationship between anxiety disorders and alcohol use disorders: a review of major perspectives and findings. Clinical Psychology Review, 20(2), pp.149–171. [online] Available at: https://www.sciencedirect.com/science/article/pii/S0272735899000276





Ready to get started?





.png)










.avif)



